Stem Cells
Stem cells” (Stem Cells or SC) are non-specialized cells, capable of dividing, simultaneously giving rise to other stem cells (equal to the mother cell) or to a terminally differentiated (mature) cell such as a hepatocyte, a specialized cell of the liver. Stem cells can be totipotent, that is, they can give rise to all the tissues of an organism, such as embryonic stem cells, or they can still be multi (or pluri) potent, which can give rise to some types of cells or tissues (adult stem cells). Essentially stem cells are classified into two categories.
The first represents the embryonic stem cells (ES Cells) found in the embryo. These are totipotent cells, that is, capable of giving rise to a complete organism starting from a single cell. Their use of is still at the center of ethical discussions today.
The second instead concerns adult stem cells (AS Cells) which provide for the maintenance of tissues and their possible repair. These cells have a particular plasticity, which allows them to differentiate into many cell types. This obviously opens interesting perspectives and very important therapeutic hopes for regenerative medicine. Among adult stem cells, those present in adipose tissue classified as mesenchymal stem cells attract particular attention among researchers, as they are pluripotent cells, i.e. capable of differentiating into different types of cells and/or tissues. Furthermore, they are adult stem cells and not attributable to the “embryonic cells” class, adipose tissue cells do not pose ethical problems.
Mesenchymal Stem Cells
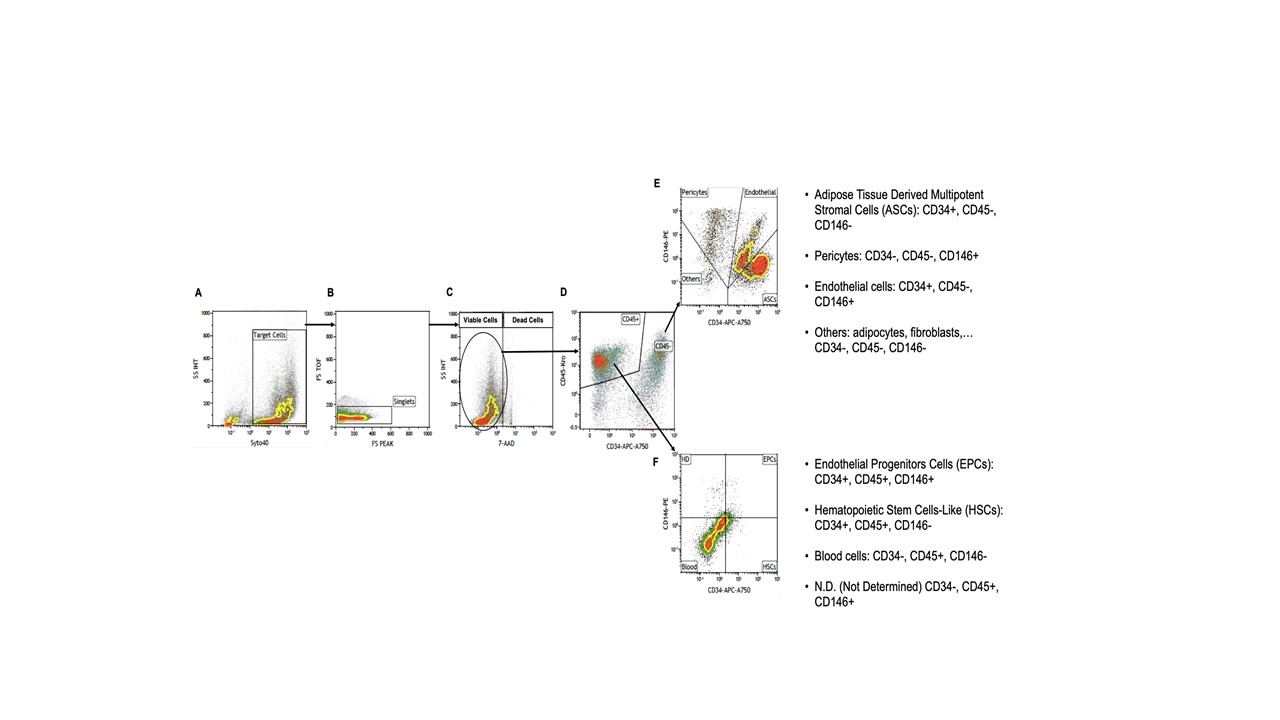
Recently, adipose tissue has attracted much interest as an alternative source, particularly compared to bone marrow, of mesenchymal stem cells (MSCs). The mononuclear portion of adipose tissue is called the stromal-vascular fraction (SVF) and contains many cell types including adipose-derived mesenchymal stem cells (ADSCs), endothelial precursor cells, pericytes, as well as, of course, adipocytes and other blood cells. as can be seen in the Figure below.
Adipose tissue cells meet all these criteria. We also consider that, with the increase in the phenomenon of obesity in modern society, subcutaneous adipose tissue has become abundant and easily accessible. To obtain adipose tissue, the liposuction technique is a procedure that is less invasive than bone marrow aspiration. In general, it can be stated that this technique produces less discomfort in the patient and does not represent a pathological condition. Small quantities of adipose tissue (100 to 200 ml) can easily be obtained by performing simple local anesthesia. Furthermore, just one gram of this tissue contains approximately 5,000 stem cells, called ASCs (Adipose-derived Stem Cells), approximately 100 times more abundant than those that would be obtained from the same volume of bone marrow. For these reasons, adipose tissue can be considered a rich resource of mesenchymal stem cells.
Therapeutic applications of mesenchymal stem cells
The speed with which stem cell research proceeds makes the boundary between what is already a reality and a therapeutic opportunity very fluid today and what will most likely be so in the very near future. The hope of biomedical research, however, is that of using stem cells as a regeneration tool for many tissues or organs. To date, many clinical studies have been carried out which have given rise to hope for the application of stem cells for the treatment of many pathologies.
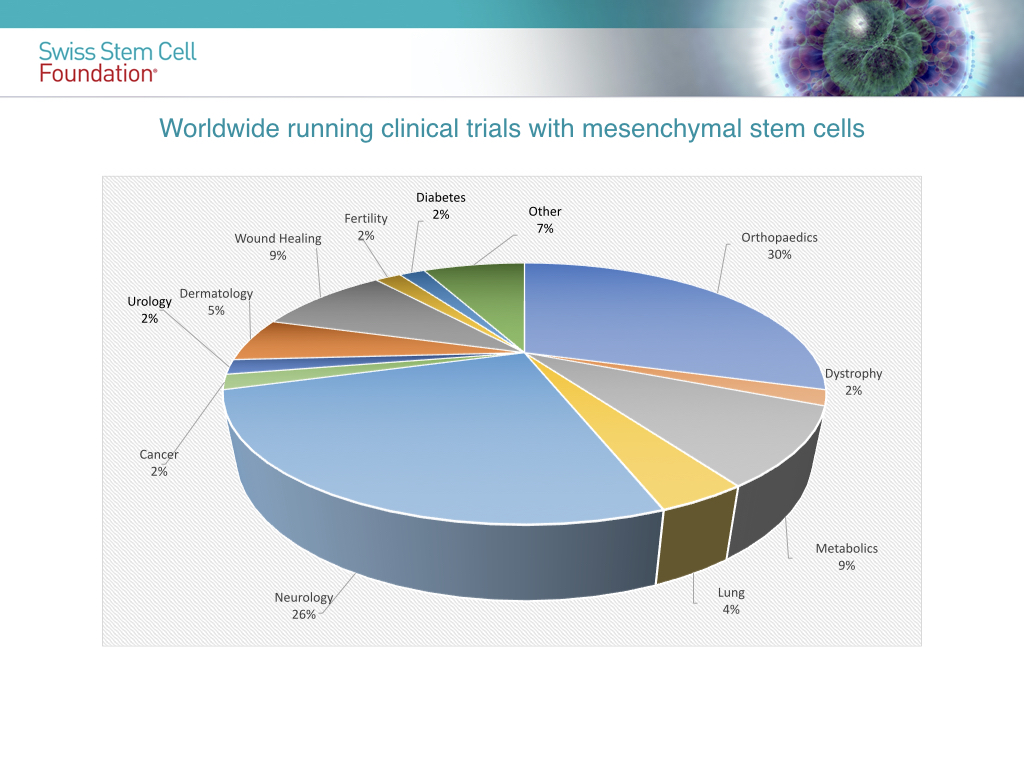
In conclusion we can say that the next few years will allow a better understanding of the biology of mesenchymal stem cells and their therapeutic action to the point of transforming cell therapy into a new clinical paradigm, allowing for better healing of many pathologies that are still incurable today.